David visited Dynamic Sports Physical Therapy in New York City and explained that he had been experiencing occasional bouts of

Throughout each day, when performing just about any given activity, we have our vestibular system to thank for keeping us

Elizabeth is a 27-year-old patient who visited Dynamic Sports Physical Therapy in New York City because she had been dealing

Many medical issues can easily be brought up to your doctor, while others might give you pause before discussing due

Fascial Manipulation is a manual therapy technique developed by Luigi Stecco, an Italian physical therapist, over the last 40 years.

When pain develops anywhere in the body, the most common approach is to address it by focusing primarily on that

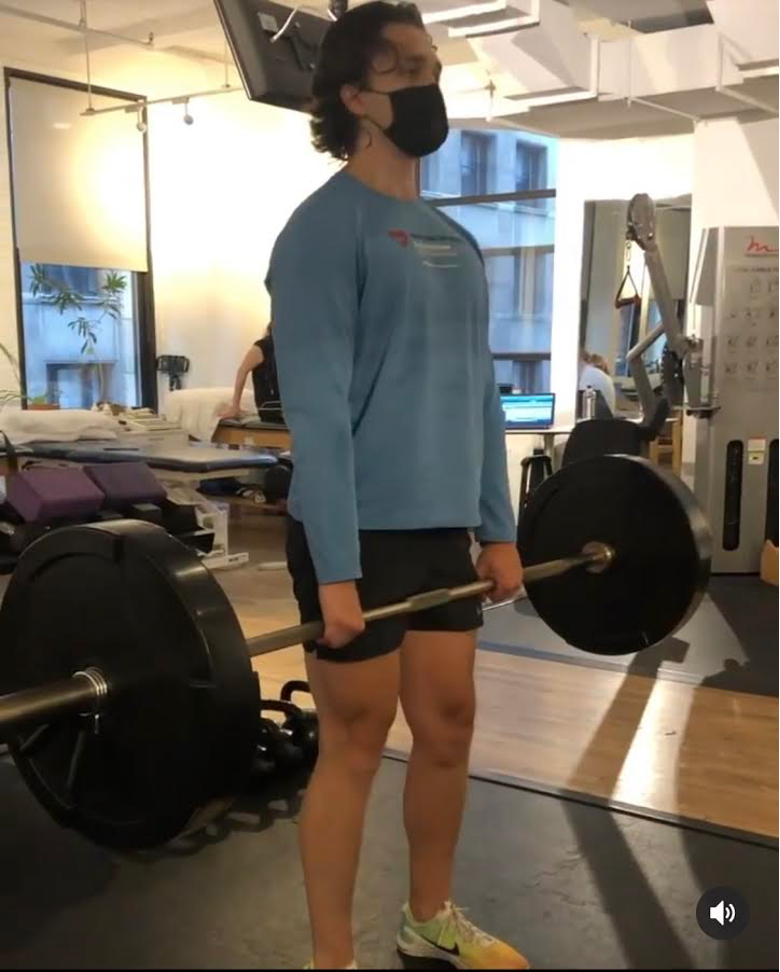
Brendan Keevan is an active 27-year-old active tore the anterior cruciate ligament (ACL) of his left knee from a non-contact
Tears of the anterior cruciate ligament (ACL) get lots of attention in sports, and there are some very clear reasons

Rose is a 50-year-old hospital administrator with a history of severe headaches. She had been previously diagnosed with migraines, and

Headaches can be relentless. For many individuals, a headache can ruin their day or even leave them incapacitated for an
